What issue can we solve for you?
Type in your prompt above or try one of these suggestions
Suggested Prompt



Health
Platforms and the Coming of Age: How to Develop the Next Generation of Platforms
Platforms and the Coming of Age: How to Develop the Next Generation of Platforms
The paradigm shifts occurring in healthcare are substantial. New ways of using data, new approaches to service design and delivery and a core belief in the renaissance of the health relationship are poised to disrupt the industry. But all this will not be possible without imagining a new platform ecosystem focused on healthcare.
The definition of “platform” to deliver these new paradigm shifts is the challenge of the next decade—to develop an ecosystem of interoperable platforms that support new ways of using data, digital-first service delivery redesign and management of digital-first healthcare relationships, all while delivering an outstanding caregiver, provider and patient experience.
If designed and delivered in the right way, this will go down in history alongside the creation of the internet. Here’s why organizations are increasing their focus on improving patient and member experiences in order to make sense of platform complexity.
Platforms, platforms everywhere and not a drop to…
Healthcare is no stranger to platforms. Particularly in the last 20 years, a wide variety of platforms have significantly influenced the experiences of patients and caregivers, as well as the work of devoted individuals providing clinical support and care daily. The patchwork of platforms includes electronic health records (EHRs), telemedicine, remote patient monitoring (RPM), clinical decision support system (CDSS), claims management, pharmacy management, health information exchange (HIE), patient portals and the list goes on. Each provides independent crucial functions and, as a collective, add to the growing complexity and weight of the ecosystem.
If you know what ARPANET stands for, chances are you’re wishing this text was bigger. ARPANET, or the Advanced Research Projects Agency Network, was the very first network of computers that gave birth to the internet, the mother of all digital platforms. It started with four West Coast computer centers being remotely connected in 1969, grew to 213 across North America and Europe in 1981, and was the basis for the launch of the internet in the 1990s. Key innovations include the interaction between communications (TCP/IP) and the user experience (HTML); in short, interoperability was a significant focus. Today, the internet is barely recognizable compared to the internet of the 1990s. The phrase “mother of all digital platforms” is intentional, as it has enabled the birth of so many new platforms, such as Google, Apple, Facebook and others.
A comparison to ARPANET is useful here. Just as interoperability innovations created a new world, many of the frustrations with EHRs are based on the lack of interoperability. According to a Stanford Medicine poll, 67 percent of primary care physicians believe that solving interoperability deficiencies should be the top priority for EHRs in the next decade. Much is being done in this area, most notably through the Fast Healthcare Interoperability Resource (FHIR) and the Trusted Exchange Framework and Common Agreement (TEFCA), along with subsequent initiatives.
Organizations have increased their focus on improving patient and member experiences in order to make sense of this complexity. How can they get out from under this weight of disconnected legacy platforms and prepare to deliver the next iteration of healthcare?
Many argue that EHRs should be the new platforms that support the next iteration, especially considering that the $100 billion spent on EHRs over the last decade has both exhausted healthcare CTO budgets and, given the price paid, should already be doing a lot more. Many are frustrated with EHRs. The Stanford Medicine poll indicated that 71 percent of physicians reported that EHRs contribute to burn out, and 59 percent believe EHRs need a complete overhaul.
It can be hard to imagine how to turn a platform with that kind of animosity into one that builds the future. But organizations are recognizing these frustrations. Epic, a vendor with over a third of EHR market share, is addressing the need for a more connected ecosystem. Efforts such as Care Everywhere and Share Everywhere have established connection points between providers. As recently as December 2023, these initiatives received a Qualified Health Information Network (QHIN) paving the way for TEFCA participation. These are some necessary and meaningful steps towards unlocking the vast amounts of data that sit within EHRs. But there is still much more work to be done.
Embracing a platform mindset
Why should healthcare organizations care about platforms? Firstly, the way other industries, such as travel, retail or banking, meet the needs of consumers is all powered by platforms. Secondly, healthcare patients expect more sophisticated digital experiences than they are receiving. Thirdly, physicians want connected care across the entire health ecosystem.
In order to improve patient and physician experience, frontline services will need to adapt and evolve. Currently, they are not set up to do so easily or quickly. This is where platforms enable new service delivery, either through personalization, optimization tweaks or more dramatic changes, allowing digital experiences to be transformed much faster and with less disruption.
Building and implementing new platforms is akin to building a plane while flying it. Ironically, this is exemplified by the airline industry's legacy platform that was overhauled without stopping operations. By the 1950s, reconciling seat inventory with reservations had become incredibly challenging. Over the next few decades, the travel industry started creating global distribution systems (GDSs) with companies like Amadeus and Sabre pioneering innovative solutions and fostering industry-wide collaboration to bring about large-scale change. These global platforms acted as a conduit for booking travel, whether it was a plane ticket or a hotel booking, providing live product, price and availability information. In essence, they are simply facilitating the exchange of data. This meant that people didn’t have to go to an American Airlines store (yes, they used to exist) to book a plane ticket; instead, they could go to a local travel agent. It meant that travelers didn’t require a travel agent to book a plane ticket, they could do so within an airline app. By the 1990s, all airlines adopted platforms that referenced inventory, passenger data and schedules, facilitating self-service and metasearch engines. Services such as Booking.com and Expedia offered cheap hotel rooms. Travel agents, airline apps and online brokers all used GDS to deliver modern travel experiences, with Sabre alone doing over 76 million plane bookings a year and more than 50 million non-airline bookings.
Travel is a great example of an industry that is meeting the needs of consumers, all powered by their travel platforms, Sabre and Amadeus. In healthcare, patients expect much more sophisticated digital experiences than they are receiving. Platforms can enable new service delivery to improve patient digital experiences more quickly and with less disruption while consistently innovating at pace.
There are a few examples of platform innovation in healthcare, such as the National Health Service (NHS) in the U.K. In order for it to work as an integrated system, it operates a number of data exchanges, including those for demographic information, appointment management, clinical summary sharing, consent management and more. This enables a seamless and connected healthcare experience across the 1,150 hospitals, 6,500 primary care clinics and 11,400 community pharmacies of the NHS. They are empowered by this underlying platform.
In the U.S. healthcare system, two dynamics are at play that relate to the creation of emerging platforms. First, there is an acceleration of hospital acquisitions, such as Risant Health or Ascension, Advocate Aurora or Spectrum Health, to name a few. Large health systems will need an integrated platform to support their organizational integration and strategic goals. Secondly, similar data exchanges are emerging as federal policy starts to push them through TEFCA and the establishment of Qualified Health Information Networks (QHINs). So, the industry can expect to see further openness on data exchanges, which will allow hospitals to create connected experiences, even beyond their own services. As a result, hospitals that have platforms, or the ability to use exchanges and platforms, will have a powerful advantage in delivering the type of experiences that customers expect and that they receive from other industries.
Four principles crucial for success
Hospitals that do well in the platform ecosystem will be those that effectively adopt a platform mindset and embrace the right architecture principles. While the specific requirements and approaches will be unique to each organization, there are a few principles that are crucial to the success of any digital transformation.
However, it’s more than just applying the right architecture principles. Modern platforms are built in a very different way compared to those of the past. Consider how skyscrapers are built. A developer will hire an architect and engineers to come up with the building design, which may be, for example, 18 stories high, with x amount of commercial space, y number of apartments and z amount of car parking. The elevator fire escape shafts will be built according to regulations, the ventilation systems will be placed on the roof and the plumbing will be structured per the specifications. It’s designed, then built, then used—18 stories, $450 million, job done. That’s how old platforms were built. New platforms are designed differently. The architect and engineers will start by focusing on the services needed (such as ventilation, plumbing and floor-to-floor access), and build a few floors. Then more floors will be built as needed. The services will be standardized, making it seamless to “move” between skyscrapers. The point is, it’s a completely different way of building things that isn’t about building a fixed system that becomes legacy technology, but rather something that is far “lighter,” more flexible and evolves over time.
The frontline challenges: keeping it real
It’s one thing to write about the future, about “what” must be built, but truth be told, the real innovations are around “how” to get there. It's worth reflecting on current state issues for healthcare organizations—issues that make digital transformation in healthcare particularly challenging. Of course, the specific circumstances for each healthcare organization have unique nuances, but generally, there are four key drivers consistently seen across healthcare organizations that have left many leaders feeling unsure of how to move forward.
Risk of disruption to daily operations
Whether it is reviewing a patient’s health history, navigating clinical workflows or processing insurance claims, platforms are supporting huge swaths of activity happening every minute within healthcare organizations. Employees have learned the capabilities—and limitations—of these platforms, passing on workarounds and precautions to new colleagues. This acceptance of the status quo isn’t due to a lack of desire for change. Rather, it’s a need to ensure that the vital services being provided are not interrupted, giving way to the old adage that sometimes, it's better to deal with the devil you know than the devil you don't.
High volumes of (sensitive) data
Over 30 percent of all data in existence today is generated by the healthcare industry, and the average hospital produces an additional 137 terabytes per day. Much of this is personal health data which comes with an additional layer of security requirements and government regulations. The management and movement of this data is an enormous task that few off-the-shelf platforms are capable of managing effectively and securely, not to mention the potential risks associated with migration. Furthermore, organizations are faced with the crucial and complicated task of thoughtfully constructing and carefully managing data privacy and consent across their organizations.
Lack of standardized structures
When each EHR is implemented, it severs ties with its mother platform and becomes a bespoke instance with its own qualities, quirks and capabilities. This can negatively impact the usability of the data it’s capable of sharing. Adherence to Fast Healthcare Interoperability Resources (FHIR) and Health Level Seven (HL7) only ensures information is able to be transferred between organizations. The Sequoia Project, recognized by the Office of the National Coordinator for Health Information Technology (ONC) as the coordinating entity for TEFCA, highlights the issue. According to The Sequoia Project, it’s one thing to get health data to the right place at the right time; it’s quite another to make sure that data is complete and useful. Without standard structures and taxonomies for all kinds of data (clinical, educational, diagnostic), there will continue to be high friction between and within healthcare organizations, inhibiting the instigation of a true platform ecosystem.
Unclear or delayed ROI
With significant capital needed to transform such large and vital platforms, organizations rightly expect to be able to quantify the impact of their investments. However, the more noteworthy results, such as lower cost to serve, higher patient satisfaction and improved health outcomes, often take a long time to be realized. Meanwhile, short-term gains like maintenance costs, increased productivity and more consumer data capture points can be overshadowed by the high degree of short-term investments and change management required to get there.
Planning the revolution
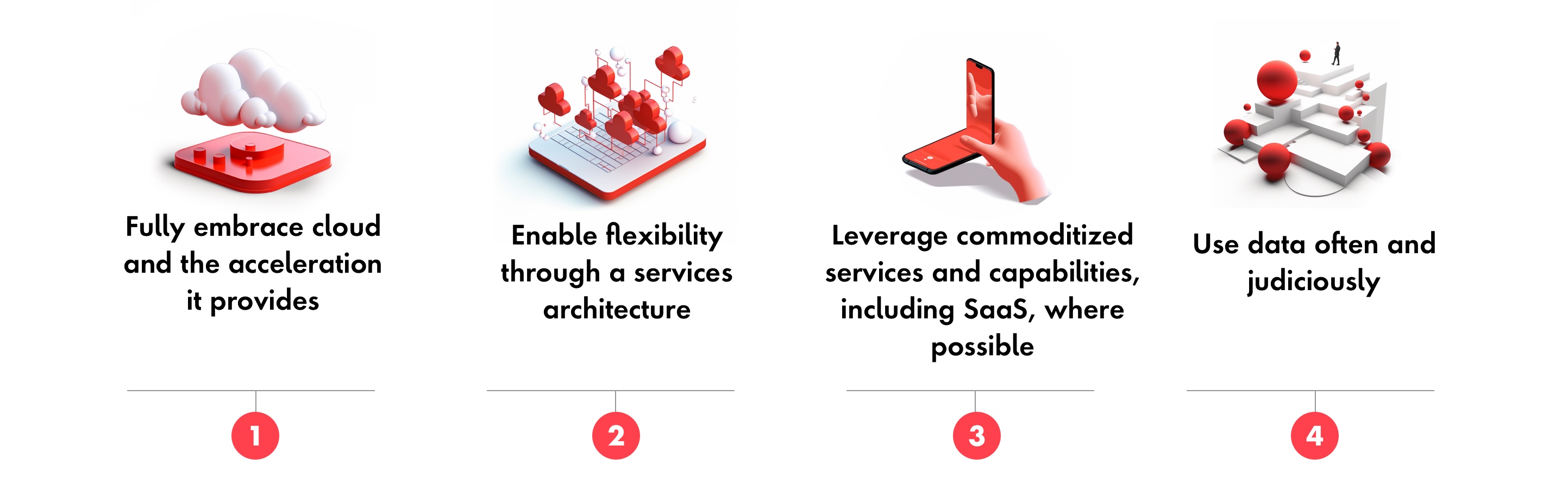
To develop the next generation of platforms, organizations must structure a two-stage plan. First, each healthcare organization needs to anchor their approach around the following four areas:
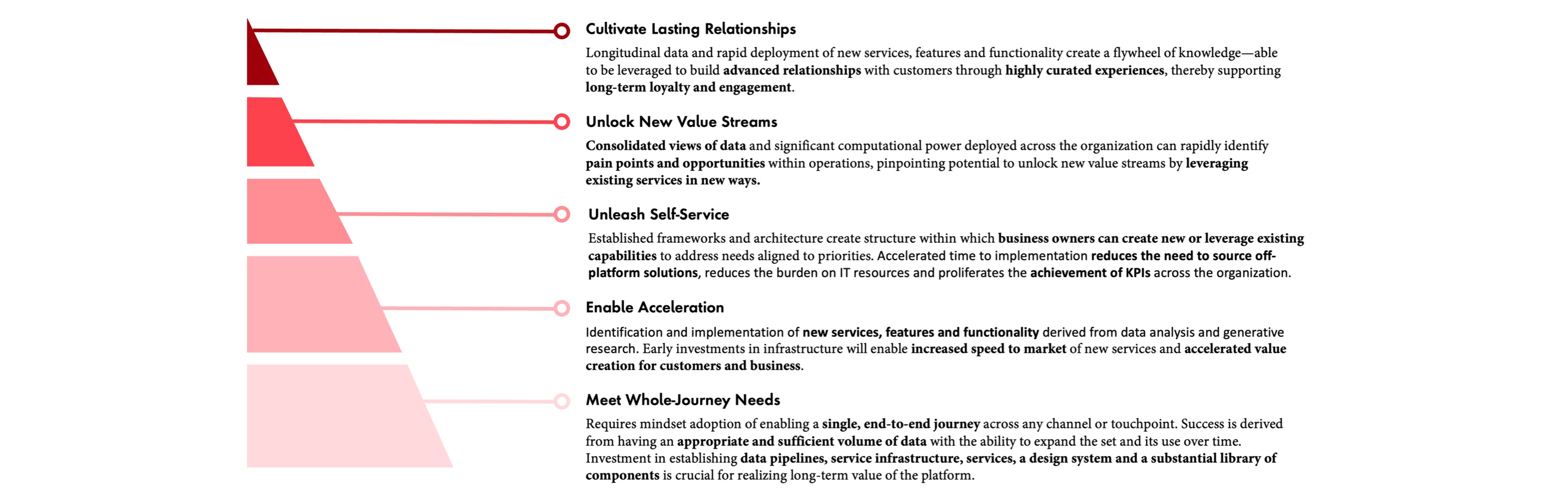
After anchoring their approach, organizations need to make strategic investments in buying, building or customizing platforms that meet their needs—a process that requires thoughtful dialogue, expertise and guidance—to create a robust foundational platform in the near term. Using the following framework as a progression tool, organizations can align investments to long-term objectives and identify new value pools these investments will unlock, resulting in accelerated growth, impact and up to 10x cost-to-value ratio over time.to create a robust foundational platform in the near term. Using the following framework as a progression tool, organizations can align investments to long-term objectives and identify new value pools these investments will unlock, resulting in accelerated growth, impact and up to 10x cost-to-value ratio over time.
Platform Value Pyramid – investment in building a robust foundation will accelerate growth, impact and up to 10x cost-to-value ratio over time
The juice will be worth the squeeze.
Embarking on transformation demands courage, knowing many organizations have struggled to innovate amidst industry disruptions. As the healthcare industry looks to embark on its own transformation, it will take similar kinds of innovation and collaboration, as well as the two-stage plan outlined above. Undoubtedly, decisions must be closely tuned to the changing policies, workforce realities and complexities of the business, but with thoughtful design and investment of future-orientated platforms, the industry can efficiently and effectively create impact at scale through digitally enabled experiences that are as dynamic as the health and lives of their users.
Related Reading
-
![]()
Insight
Reimagining Healthcare Experiences with Generative AI
Learn how artificial intelligence can elevate patient interactions and automate processes within provider, payer and pharmaceutical organizations.
-
![]()
Insight
The Post-Covid Patient-Centric Transformation
After the pressure of the pandemic, here’s how life sciences organizations can use digital to maintain lasting change and resiliency.
-
![]()
Insight
Pharma Growth–Mining Opportunity from Our New Virtual World
In a world radically transformed by COVID-19, pharmaceutical sales have moved out of conference rooms and now faces an unfamiliar environment where HCP and Consumer engagement and decisions are increasingly occurring in virtual spaces. Learn more here.







