What issue can we solve for you?
Type in your prompt above or try one of these suggestions
Suggested Prompt



Health
How Healthcare Service Delivery Can Be Reimagined
How Healthcare Service Delivery Can Be Reimagined
There’s been no shortage of investments in healthcare startups and digital health in the last decade. Despite the numerous ones that have failed, there seems to be a belief that new entrants may be the way to transform the industry. And yet, the trend in these investments hasn’t made a meaningful impact on how people feel about healthcare.
What is getting in the way of scaling the work of startups and enabling established organizations to be the source of innovation?
Healthcare is different
In any industry, startups are fertile ground for solving entrenched problems. Often, they use a “fresh pair of eyes” to spot friction and frustration in the system, thoughtfully design products and services that address those and raise the bar on what established entities need to do to evolve. In many cases, the established entities—especially those who have made wise investments in digital transformation—adapt and adopt these new ways of doing things and establish them as the norm.
In healthcare, too, startups are solving some of the stickiest problems that have long plagued the industry, such as friction-free digital communication with care teams, reduction in repetition of giving information and making preventative care easier to engage with. But the conversion of startup ideas into the norm is where things seem to stall. Established providers, payers and the like have not been able to adapt in ways that allow them to be the fertile ground of innovation. And startups have struggled to move from their microcosms of impact to scaled services being delivered through the broader health ecosystem.
The healthcare experience: a leap of faith
For more than a decade, the healthcare industry has looked to other industries, such as retail, to mentor its approach to health. It’s time to acknowledge that this hasn’t worked and that it is inappropriate. The focus on the “consumerization” of healthcare has distracted from true digital transformation.
Consider Amazon, who consistently ranks either number one or near the top in retail satisfaction. They have achieved this for three reasons: clear and wide product selection, affordability and speed. It’s a service that obsessively makes things convenient, and when they make a promise, they keep it. That’s a strong consumer experience. But the comparison to healthcare is flawed. Top-line outcomes in healthcare cannot be guaranteed. In fact, when placing a consumer lens on the healthcare service, the paradigm breaks down instantly.
People often enter healthcare services as follows:
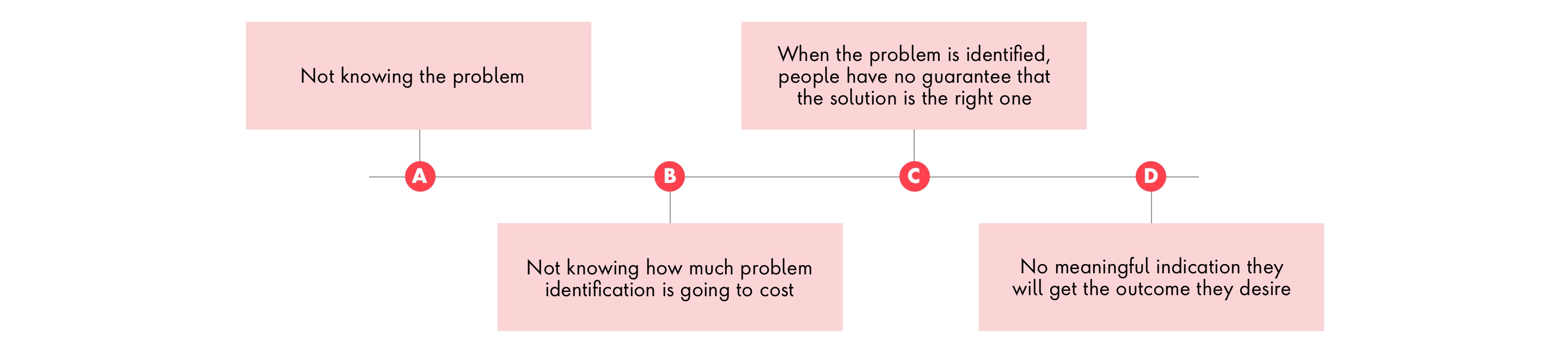
Healthcare is not a consumer experience. It’s a highly calculated leap of faith. This last point is one of many issues that make healthcare different and tricky. It’s one of the reasons Big Tech has struggled to make an impact. It’s true that patients do experience good consumer experiences in other sectors such as banking, retail and travel; they know what “good” looks like, especially in the digital space. Healthcare can learn from some best-in-class digital best practices but must recognize that it doesn’t always directly transfer to healthcare. Healthcare is different.
To create a healthcare system that works well, the system must be designed to work well. This means letting go of some “anchor points” and understanding that the next generation of healthcare services requires a rethink with the patient as an independent self, choosing the healthcare experiences that fit them.
Reimagining the patient experience, step by step
Adopting a patient-led approach to create a better U.S. healthcare system starts by seeing the patient (self) as an independent being. The next step is to design the system with patients at the heart. This isn’t just about the Orbital Care concept of healthcare relationships—this is about the fundamentals of healthcare design. We need to rethink three areas, or anchor points, in order to improve the U.S. healthcare system.
What good services look like
If this all sounds dramatic and perhaps pessimistic, then it’s time to adjust the balance. There are plenty of reasons to be excited about redesigning healthcare services so that they intuitively become part of a vastly improved healthcare system. There are best-in-class examples from both established organizations and startups. Here’s where and how this is happening.
Align to health and life context
Rather than focusing on the triage-like nature of hierarchical care, we are seeing interesting advances begin to focus on why people are seeking care and type of the care they need. Galileo Health, for example, is restructuring care delivery It supports patients using three mental models of care. These include “everyday care” (for common medical issues such as referral requests, prescription renewals, birth control selection and PrEP), “getting answers” (for determining what’s behind symptoms such as headaches, bloating, fatigue or back pain), and “ongoing care” (for data-driven management of conditions such as asthma, diabetes, acid reflux and anxiety). This approach also addresses the realities of accessing care. Galileo amasses the right group of individuals virtually to address the holistic needs of its patients, bringing care into the home when needed, and utilizing care at a distance (clinic-based or hospital) as a last resort rather than the default.
Design services with digital-first interactions
Organizations that are thoughtfully deploying digital tools and experiences are delivering strong mutual value in care delivery, aligning to patient expectations and creating efficiencies for care teams. Providers like One Medical set out to rethink primary care by considering the roles and infrastructure needed to support digital-first interactions. Practitioners like Dr. Tom Lee also took care to immerse themselves in each role to acknowledge how people underestimate how hard it is to execute services. This analysis yielded insight into how to reduce friction for historically frustrated patients.
Of course, One Medical has all the expected digital capabilities, such as online booking and health records, scans and vitals, in one place. But it stands out for its redesign of “back of house,” delivering near-immediate response times, real-time care coordination and, more recently, a seamless link between medication management and supply delivery. No wonder Amazon acquired them.
Make physical experiences frictionless
Care provided in person will continue for the foreseeable future, and with that comes the continued opportunity to reduce frustration and inefficiencies in those experiences.
Focus on the outcome and rethink how to get there
Operational procedures and workflows serve as a blueprint for delivering quality care with consistency. But when resource constraints inhibit the ability of providers to deliver quality care, the need arises for novel approaches to achieve the same outcomes. When organizations create frameworks for care, it invites creativity in designing new ways to deliver it. One such example of innovation from the inside out comes from Mississippi. With a significant portion of their patient population living in rural areas with limited access to expert acute and specialty care, the University of Mississippi Medical Center (UMMC) regularly saw an influx of patients needing to be transported from local care facilities—a costly and risky endeavor—or traveling long distances to receive more advanced care.
The strain on the system was unsustainable, and new funding sources were unlikely to increase the volume of expertise and equipment needed to support these far-reaching communities. Starting as a pilot program and quickly expanding to be a core part of UMMC care delivery, the clinical operations teams devised a “hub and spoke” model for connecting local providers with experts at the main hospital in Jackson. This solution not only leaned into a paradigm that thought differently about physical space but also delivered meaningful results, with significant gains in diverting patients from the ER and a positive impact on health outcomes in disease states such as diabetes.
Use data to increase engagement to improve outcomes
Services that understand the lived experiences of users, investigate the barriers to their health challenges and design solutions that clearly and quickly address those issues while recognizing the complexity of care delivery will be the ones that will persist and produce sustained impact.
Devoted Health is one of the few health plans to achieve a five-star rating from CMS in 2023 and strongly believes in the power of primary care. However, it acknowledges that the current approach in the U.S. isn’t working and that most emerging solutions are either insufficient in scope or take too long to deliver measurable impact. So, they set out to design a vertically integrated health organization from the ground up that could augment the work of over-extended PCPs and support improving the lives and health of Medicare Advantage patients. They have certainly delivered on that promise, reducing A1C levels by 2.1 in 84 days on average, lowering systolic blood pressure by 15 points in 40 days, achieving 90 percent medication adherence and lowering readmission rates by 38 percent.
But it is the trust they have built with members and care teams that is driving the longitudinal relationships and sustained results. Almost exclusively through virtual means, new members go through an initial health assessment appointment that typically lasts an hour, giving the patient and provider ample time to get to know one another and build rapport. These conversations are structured with pre-appointment questionnaires and in-appointment frameworks such as the Patient Priorities of Care guide. These conversations not only serve as the connection point to the vast pool of services (16 robust service lines and growing) but also ensure that individualized care plans center around what matters most to the patient. Often, those outcomes sound more like “having my knee stop hurting so I can play with my grandkids” or “feeling less tired so I can still work and support my spouse who has dementia.”
Success is not only achieved by the design of service enablers but also by the creation of aligned care plans. The Devoted Health single software platform powers everything they do, removing data silos, enabling workflows and more. Instead of taking a technology-first approach, they utilize those tools to effectively optimize the work of care teams. Data scientists and software engineers shadow care teams to observe the work firsthand and call out opportunities where technology could expedite or eliminate a task rather than forcing care teams to operate in new ways. But perhaps the most fundamental difference is the three guiding principles they apply to everything they develop—practicality, humility and love.

Getting healthcare innovation to scale
The stand-out examples above are great services designed by great people, but it’s still a struggle to embed this mindset into the mainstream. The focus now needs to shift towards proliferating these ideas across the healthcare system with the aim of creating a large-scale shift in the modus operandi that preserves the solvency of providers of care and accelerates the impact for those receiving care. From an outside perspective, it can be difficult to understand why this poses such a challenge, considering the spend on healthcare at the federal level alone. However, the comparison to other countries is unfair for one simple reason: unlike the other 10 countries, the U.S. healthcare system has never been explicitly designed as a cohesive system. As Dr. Tom Lee, founder and CEO of Galileo Health, puts it, “It’s a patchwork of a lot of different well-intentioned initiatives, well-intentioned organizations trying to do things within those constraints.” Its interconnectivity and universality are an afterthought to the creation of healthcare organizations, where silos are literally built in.
Comparing the U.S. healthcare system to that of other countries is not a productive activity. That said, the U.S. healthcare system faces a unique opportunity to solve its systemic issues, not by replicating structures of others that focus on managing millions of individuals, but through empowering each individual to be the center of their healthcare system and enabling them to navigate the services of the system, without the system getting in the way. Here are three key imperatives for enabling innovation and accelerating transformation of service delivery at scale.
Embrace silos but create connection hubs
The complexity of healthcare necessitates a high level of specialization to deliver care across the continuum. However, this often leads to silos and fragmentation. To counterbalance this, successful organizations are finding ways to facilitate deep and meaningful connections between specialties, enabling innovative resource management. One of the best examples of this approach is on a small island off the coast of England. With a population of 140,000, the Isle of Wight has almost double the U.K.’s national average of people aged over 65. Given the concentration of health and social service needs for this population, many of whom are isolated from family who live on the mainland, the deployment of crisis services is vital to the health of the island.
A difficult snowstorm in 2010 led to a light-bulb moment, and the island completely reorganized how it deployed health and care service personnel. By housing emergency call operators, NHS call handlers, paramedics, social workers, pharmacists and even a home alarm company in an integrated hub inside St. Mary's Hospital, it became the central hub of the emergency and unscheduled care system. Placing people from every service within feet of each other allows for constant communication and has continued to promote innovation and resource deployment.
Based on its unique view of patient services, the Isle of Wight joined the National Digital Twin Programme in 2022 to expand its ability to predict and respond to needs and effectively deploy resources for the benefit of society.
Close care gaps through partnerships
Some of the biggest issues facing healthcare—be it access, equity, cost or outcomes—are being addressed by startups focused on solving specific issues. These services tend to be digital-first, but their digital focus is matched by their clinical thoroughness and design of new, more effective clinical protocols. Take women facing health issues related to menopause, for example. To support the 57 million women of menopause age in the U.S., there are only 500 practitioners registered in the U.S. that are certified by the North American Menopause Society (NAMS). They often endure long waits for appointments and receive subpar care. Midi is an example of a virtual care clinic addressing menopause healthcare with a particular focus on maximizing the value of virtual care. Through research and feedback, Midi discovered that the key to successfully crafting a care plan is listening.
“We need to understand what’s going on in their bodies. And that takes listening. It actually doesn’t take looking at your body at all—it takes looking at your facial expressions and understanding the emotional things that are going on.”
Joanna Strobe , Founder of Midi
Telehealth is an ideal modality for engaging in just that. Clinicians review patient-provided answers to an extensive pre-visit assessment, after which the platform dynamically recommends questions and protocols to be followed during the telehealth consultation. According to Midi founder Joanna Strober, menopause healthcare can be better provided by telehealth than in person.
The thoughtfully designed service experience addresses a clear insufficiency in the system and has become an attractive way for established organizations such as Memorial Hermann and Lifepoint Health to meet long-standing needs of their patients through a partnership with Midi, integrating their services into the suite of options available to their patients.
“It’s a different relationship when you’re talking to someone [via telehealth] than it is when you go to a doctor’s office, and you’re sitting on a table and asked to take off your shirt. You don’t feel like talking about these things at that point. You just want the visit to be over.”
Joanna Strober , Founder of Midi
Pool and distribute resources
Thin margins and persistent labor challenges plaguing providers mean judicious use of resources is crucial for survival. Many of the more recent mergers and acquisitions in the industry have cited service expansion and economies of scale as reasons for the deals. The work of bringing these ambitions to bear relies on looking for opportunities to leverage existing resources across a network, rather than duplicating them throughout. Those who are succeeding are looking at past examples, such as the hub and spoke model put in place at UMMC, for inspiration. Rather than waiting for funding and resources to add clinical expertise to all rural community hospitals in their network, UMMC connected those hospitals to experts in their main hospital via remote consultations, thereby maximizing their existing resources. Others are taking more novel approaches to distributing resources. Risant Health, for example, is stitching together hospital systems in a different kind of agreement, allowing entities to retain elements of their identity and operations while centralizing best-in-class tools, data insights and population health management approaches into a unified platform in service of improving outcomes.
The digital health revolution is here.

Only when healthcare organizations begin the work of designing with these examples and imperatives in mind can a unique U.S. healthcare system that’s centered around unique individuals be formed. The healthcare system of the future will be accessible to many more people, cost less and create better outcomes for each individual, thereby elevating the U.S. healthcare system on a global scale.
Related Reading
-
![]()
Insight
Reimagining Healthcare Experiences with Generative AI
Learn how artificial intelligence can elevate patient interactions and automate processes within provider, payer and pharmaceutical organizations.
-
![]()
Insight
The Post-Covid Patient-Centric Transformation
After the pressure of the pandemic, here’s how life sciences organizations can use digital to maintain lasting change and resiliency.
-
![]()
Insight
Pharma Growth–Mining Opportunity from Our New Virtual World
In a world radically transformed by COVID-19, pharmaceutical sales have moved out of conference rooms and now faces an unfamiliar environment where HCP and Consumer engagement and decisions are increasingly occurring in virtual spaces. Learn more here.







